Su Lab
- Research
- Lab Members
- Publications
- Contact Us
Nearly 60,000 girls, adolescents and young adult women are diagnosed with cancer each year. More than ever, young people will survive cancer and can look forward to the future. Cancer treatment can affect future fertility, pregnancy and the menopause. Currently, there is limited information to help young survivors, their families and their healthcare providers navigate these complex issues. Our research group conducts observational and interventional studies to help young cancer survivors improve their reproductive health.
Fertility preservation care before cancer treatment (i.e., infertility risk counseling and fertility preservation services such as oocyte and sperm freezing) is an evidence-based practice that effectively decreases infertility after cancer. In response to cost barriers that contribute to low utilization and financial burden and distress, a number of U.S. states recently passed benefit mandate laws requiring health insurance plans to include fertility preservation benefits, with additional state and federal legislation pending. These health policies may have substantial impact on preventing infertility and mitigating medical financial hardship, but clinic and patient stakeholders report that mandated benefits are not reaching cancer patients. Leveraging implementation science methods, we are studying how contextual factors in and across the multiple levels (state regulators, insurers, health systems, and clinics) that are engaged in implementing a health policy can inform the generation of novel strategies to increase access to fertility preservation and decrease adverse clinical outcomes and financial hardship in AYA cancer survivors.
At the intersection of oncology and fertility, oncofertility care is the evidence-based practice of discussing reproductive risks with newly diagnosed cancer patients and supporting shared decision-making on FP services. Despite longstanding clinical guidelines, oncofertility care uptake is low because we currently lack scalable interventions to support its implementation in adult and pediatric cancer care settings. Drawing on implementation science, our team undertook development, usability testing, pilot testing and tailoring of the multi-component telehealth oncofertility care (TOC) intervention (pronounced ‘talk’) for diverse health care settings that care for AYA cancer patients. We are currently undertaking a cluster randomized trial across health systems to test the effectiveness and study the implementation of the intervention.
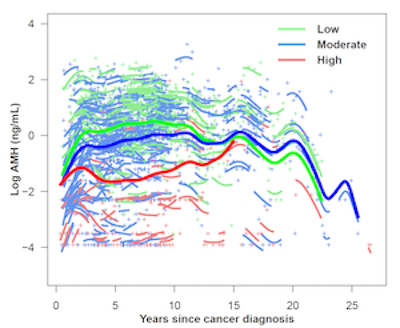
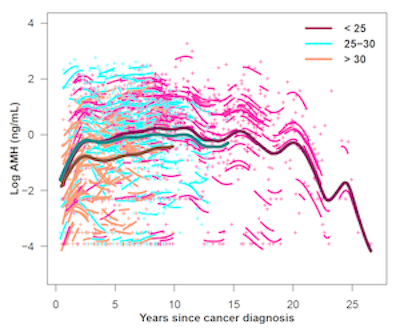
Many young cancer survivors will experience shortened reproductive lifespans, infertility, and/or primary ovarian insufficiency due to gonadotoxic cancer treatments. The window of ovarian function remaining after cancer treatment is clinically important for fertility and contraception care. We have used anti-mullerian hormone (AMH), a well-characterized biomarker of ovarian aging in women without cancer, to characterize the trajectory of ovarian function in cancer survivors. In prospective cohort studies, we have collected blood, dried blood spot, and saliva biosamples from over 1,500 young survivors.
We have shown that AMH levels fall acutely with gonadotoxic cancer treatments. Following low or moderately gonadotoxic treatments, AMH levels increased over 2–3 years and plateaued over 10–15 years before declining. In contrast, following highly gonadotoxic treatment, AMH levels were lower overall and declined shortly after peak at 2–3 years. Our next goal is to harness big data to estimate ovarian function trajectories by specific cancer treatments, in order to inform clinical counseling and fertility preservation decisions.
Most young cancer survivors undergo chemotherapy and/or endocrine therapy, treatments that impair ovarian function and result in significant reproductive health late effects. These late effects include symptoms of estrogen deprivation such as hot flashes, fertility concerns, limited contraception options and sexual problems. Together they have a major, negative impact on quality of life. Despite substantial research, treatment guidelines and clinical expertise on these issues, most young survivors and their healthcare providers have limited guidance on how best to manage these reproductive health late effects. We have developed and refined a web-based survivorship care plan on reproductive health for young breast cancer survivors, based on best evidence. This web-based intervention, tested in a clinical trial, improved infertility concerns, but did not show effect on hot flashes, contraception and sexual health.
Our ongoing projects will improve the health literacy of our breast cancer intervention, with translation and cultural adaptation to Spanish; design web-based reproductive risk summaries; generate risk-stratified survivorship care plan for adolescents and young adult survivors.
We have partnered with cancer advocacy and care organizations including Young Survival Coalition and Cancer Resource Center of the Desert for this work. Most recently, we have initiated implementation science studies on fertility care.

